gu
Table of Contents
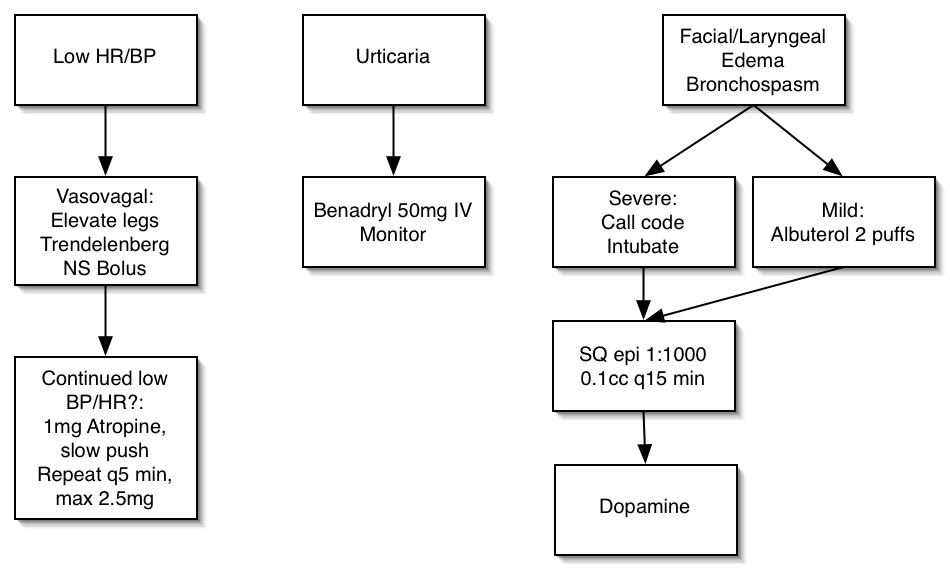
Contrast Rxn
Pelvis
Anatomy
- Extraperitoneal cavity: contiguous with retroperitoneal space
- Retropubic space of Retzius: contiguous with posterior pararenal space + extraperitoneal fat
- Perineum: below pelvic diaphragm
- Parametrium: contained within broad ligament
- Denonvillier’s fascia: positioned between prostate and rectum
Kidneys
- Combination of coritcal & medullary nephrocalcinosis suggests primary oxaluria
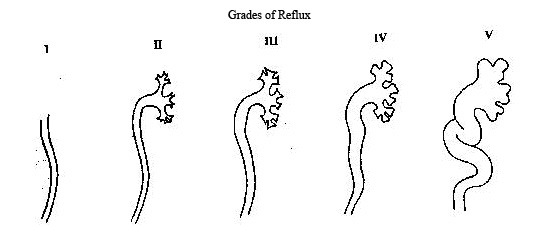
Grades of Vesicoureteral Reflux
Cortical Nephrocalcinosis (COAG)
- Cortical Necrosis (Acute)
- Oxalosis
- Alport Syndrome
- Glomerulonephritis (Chronic)
Medullary Nephrocalcinosis (MARCH)
- Medullary Sponge Kidney
- Alkali Excess
- RTA (Type 1, Distal), Renal Medullary/Cortical Necrosis
- Chronic Glomerulonephritis
- Hyperoxaluria, Hypercalcemia (Hyperparathyroidism), Hypercalciuria
Papillary Necrosis (POSTCARD)
- Pyelonephritis
- Obstruction
- Sickle Cell
- TB/Trauma
- Cirrhosis
- Analgesic Nephropathy
- Renal Vein Thrombosis
- Diabetes
Diffusely Hyperechoic Kidneys (HIV MAN)
- HIV
- Inflammation
- Glomerulonephritis
- HTN, DM
- Vascular
- SLE / Vasculitis
- Multiple Myeloma
- Acute Tubular Necrosis / ARPCKD
- Nephrocalcinosis
- ESRD
- Hemolytic Uremic Syndrome
Bilaterally Enlarged Kidneys (TIM VPC)
- Tumor
- Leukemia / Lymphoma
- Myeloma
- Inflammation (acute)
- Glomerulonephritis
- Interstitial Nephritis
- ATN
- Metabolic
- Amyloid
- Diabetes
- Gaucher's
- Acromegaly
- Vascular
- Bilateral renal vein thrombosis
- Polycystic Kidney Disease
- Collagen Vascular Disease
Bilaterally Small Kidneys (IR RAS)
- Inflammation (chronic)
- Pyelo, Glomerulonephritis, Interstitial Nephritis
- Reflux (chronic infection)
- Bilateral renal artery stenosis
Unilaterally Small Kidney (VOX HS)
- Vascular (RAS / RVT)
- Obstruction
- XRT
- Hypoplasia
- Subcapsular hematoma (chronic)
Urethral Stricture
- iatrogenic
- post-infectious (gonococcal or non-gonococcal)
- non-infectious irritation (chemical or Reiter's)
- traumatic injury
- neoplasm (long, irregular stricture ± fistula)
Bosniak Classification
- Category I - No atypical features
- US - anechoic without internal echoes, with good thru transmission and a barely perceptible but well defined wall
- CT - fluid density, no enhancement and imperceptible wall
- Category II - homogeneously hyperdense cyst that is not enhancing, or thin (<1mm) septations or thin wall Ca+
- must be 3 cm or less in diameter, have one quarter of its wall extending outside the kidney so the wall can be assessed, and be nonenhancing after contrast material is administered
- Category IIF - minimally complicated cysts that need follow-up
- not well defined by Bosniak but consists of lesions that do not neatly fall into category II
- have some suspicious features that deserve follow-up up to detect any change in character.
- Category III - true indeterminate cystic masses that need surgical evaluation, although many prove to be benign
- thicker septations or multiloculated, coarser Ca+ or solid component that is not enhancing
- may show uniform wall thickening, nodularity, thick or irregular peripheral calcification, or a multilocular nature with multiple enhancing septa
- hyperdense lesions that do not fulfill category II criteria are including in this group.
- Category IV - needs nephrectomy
- nonuniform or enhancing thick wall, enhancing or large nodules in the wall, or clearly solid components in the cystic lesion
- enhancement of at least 10 HU
RCC Staging
- Stage 1 → confined by renal capsule (completely in kidney)
- Stage 2 → beyond capsule but confined within Gerota’s fascia
- Stage 3A → extension to renal vein or IVC
- Stage 3B → positive lymph nodes
- Stage 3C → both venous extension and adenopathy
- Stage 4A → grows through gerotas fascia into adjacent organs (other than adrenal)
- Stage 4B → distant mets
Grading of Renal Lacerations

Ureter & Bladder
DDx Small Bladder (CITRUS)
- cystitis cystica
- interstitial cystitis
- TB
- rads
- unused bladder
- surgery and schistosomiasis
DDx Pear-shaped Bladder (CILLI)
- Collection - urinoma, hematoma, abscess
- IVC obstruction
- Lymphoma / adenopathy
- Lipomatosis
- Iliopsoas hypertrophy
DDx for ureteral filling defects
- Fungus ball
- Ureteritis cystica → epithelial/ subepithelial cysts due to inflammation or irritation (metaplasia of Brunn’s nests)
- Clot
- Fibroepithelial polyp
- Endometriosis
- Stone / Sloughed papilla
- Tumor / TB
- Leukoplakia: associated with Schistosomiasis; premalignant → squamous cell carcinoma
- Malakoplakia: chronic gram (-) infection (E. coli #1); ↑ DM → foamy macrophages (Hansemann) with PAS (+) inclusions (Michaelis-Guttman bodies); raised yellow lesions
- looks like ureteritis cystica
DDx hemorrhagic cystitis
- viral and bacterial infection
- drugs - cyclophosphamide (cytoxan)
- eosinophilic
- cystitis cystica
Pseudodiverticulosis
- 1-3 mm outpouchings
- DDx → calculi / infections / CA (#1 = TCC)
Ureteral TCC
- Risks: azo-dyes, cyclophosphamide, phenacetin
- Radiographic:
- “Wine glass/goblet” deformity (dilated distal ureter)
- Bergman sign (coiled retrograde catheter)
Ureteral displacement
- Distribution:
| Medial | Lateral | |
|---|---|---|
| Above Pelvis | Retroperitoneal fibrosis Retrocaval ureter (right; at L3) | Psoas hypertrophy LAD AAA Central tumor |
| Below Pelvis | Pelvic lipomatosis Iliac LAD/ aneurysm Iliopsoas hypertrophy Hutch diverticulum | Fibroids Ovarian masses |
- Medial
- Retroperitoneal fibrosis: drugs (methylsergide, ergotamine); XRT; prior surgery; malignancy; connective tissue disorders
- Retrocaval ureter (right only)
- Pelvic lipomatosis: ↑ black males; “tear-drop” or “pear”-shaped bladder; associated with ureteritis cystica
- Other: hematoma; iliac LAD or aneurysms; adnexal mass; surgery
- Lateral:
- AAA
- LAD; psoas hypertrophy
- Central pelvic mass
- Retroperitoneal fat (≠ pelvic lipomatosis)
DDx for ureteral stricture
- Infection: TB; Schistosomiasis; abscess; fistula
- CA: metastases; local extension; TCC; lymphoma
- XRT
- Inflammation: calculi; instrumentation; stent; endometriosis
DDx for ureteral dilatation
- Obstruction
- Reflux
- Primary megaureter (“beak” sign)
DDx for bladder filling defects
- Tumor: TCC; adenocarcinoma; squamous cell carcinoma; metastases (pheochromocytoma)
- Extrinsic masses: BPH; uterus (fibroids); etc.
- Other: calculus; thrombus; ureterocele (pseudoureterocele due to inflam/ tumor); foreign bodies
Hutch Diverticulum
- adjacent to UVJ; ↑ vesicoureteral reflux
Bladder Carcinoma
- Clinical: transitional cell (90% malignant); risks = azo-dyes; phenacetin; cyclophosphamide; focal thickening of bladder wall; perivesical spread; LAD (> 10 mm)
- Staging:
- Stage A: limited to mucosa + submucosa
- Stage B1: superficial muscular layer
- Stage B2: deep muscular layer
- Stage C: perivesical fat
- Stage D: seminal vesicles, prostate, or rectum
Bladder Trauma
- Contusion: interstitial
- Extraperitoneal: due to pelvic fracture, dissection into retroperitoneum + scrotum + thigh
- Intraperitoneal: usually blunt trauma with distended bladder; DX requires adequate bladder distention (> 250 ml)
DDx for Bladder Ca2+ (SCART)
- Schistosomiasis (↑ squamous cell carcinoma)
- CA; cyclophosphamide (cytoxan); calculus
- Alkaline encrusting cystitis
- Radiation
- TB
Urethra
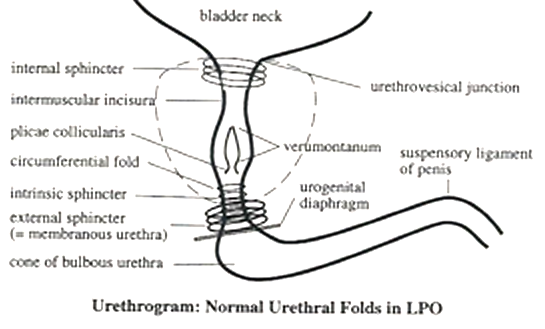
Urethral Anatomy
Anatomy (male)
- Anterior = penile + bulbous (penoscrotal junction)
- Posterior = membranous (between inferior margin of verumontanum + tip/ cone of bulbous urethra) + prostatic
- Cowper’s glands: contained within membranous urethra with ducts entering the bulbous urethra
- Glands of Littré: located primarily along dorsal penile urethra → infections (gonococcus; chlamydia)
Urethral Injuries
- Clinical: risks = pelvic trauma (especially multiple pelvic fractures); absence of blood at meatus does not exclude urethral injury → RUG
- Subtypes:
- Type I: posterior urethra stretched
- Type II: posterior disruption (above urogenital diaphragm)
- Type III: anterior + posterior disruption
- Type IV: bladder neck injury with extension to urethra
- Type IVa: periurethral extravasation with intact urethra
- Type V: anterior disruption (“saddle” injury); ↑ bulbous urethra
Female Urethral Diverticulum
- Clinical: most often acquired due to infection of Skene’s glands; ↑ posterior wall; SXS = dysuria + dribbling + dyspareunia (3 D’s);
TX = surgical resection (diverticulectomy)
- Radiographic: focal outpouching along posterior urethra; impression along inferior bladder (= “male prostate”); best seen on MRI
- Complications: infection; calculi; CA (squamous cell)
DDx for Urethral Strictures (TIICB)
- Trauma
- Inflammatory; infections (prostatitis; phlegmon; etc.)
- Calculus
- BXO (= balanitis xerotica obliterans): variant of lichen sclerosis et atrophicus (white plaques) → phimosis/ meatal stenosis; premalignant (penile squamous carcinoma)
Hypospadias
- ↑ cryptorchidism (30%) + inguinal hernias (10%)
DDx for Urethral Tumors
Benign
- Fibroepithelial polyp: solitary; pedunculated; attached near veru montanum; ↑ child/ young adult
- Transitional cell papilloma: ↑ prostatic/ bulbomembranous urethra; ↑ bladder papillomas; older adults
- Adenomatous polyp: ↑ young men; adjacent to veru montanum
- Penile squamous papilloma / condyloma acuminata: verrucous lesion in penile urethra; associated with cutaneous disease
Malignant
- Squamous cell carcinoma (70%): distal 2/3 of urethra; risks = venereal disease; ↑ stricture (> 80%)
- TCC (10-20%): posterior 1/3 of urethra; ↑ multifocal
- Adenocarcinoma (10-20%): arise from periurethral glands (Skene; female) and glands of Cowper/ Littré (male)
Testes
Testicular Cancer
- Clinical: seminomas → orchiectomy + XRT; nonseminomas (radioresistant) → orchiectomy + chemotherapy
- Staging:
- Stage I: limited to testes and spermatic cord
- Stage II: lymph nodes below the diaphragm
- Stage III: lymph nodes above the diaphragm
- A: lymph nodes only
- B: extranodal mets
- Lymphatic spread: along gonadal veins → renal hilar nodes; external iliac nodes → para-aortic nodes
- Hematogenous spread: uncommon except for choriocarcinoma
- Cryptorchidism: located from inferior renal pole to superficial inguinal ring; ↑ risk of torsion (↑ 10x) + malignancy (↑ 50x); usually atrophic
Extratesticular Mass DDx
- Inguinal hernia
- Inflammatory mass such as infection, sarcoidosis
- Benign neoplastic processes such as adenomatoid tumor, epidermoid inclusion cyst
- Malignant processes such as soft tissue sarcomas, mesothelioma of the tunica, lymphoma, and metastatic disease.
Peyronie's Disease
- Calcification of tunica albuginea of corpora cavernosa
- Idiopathic, older men (> 45 yrs old)
Prostate
Anatomy
- U/S → hyperechoic central gland = transitional + central zones
- Transition zone (5%): periurethral → BPH
- Central zone (25%): ejaculatory ducts
- Peripheral zone (75%): carcinoma (> 80%); hypoechoic
BPH
- periurethral transitional zone; enlarged, lobulated gland; cystic degeneration; Ca2+; elevation of bladder base; bladder wall thickening and trabeculation
Prostatic Cysts
- Midline:
- Mullerian duct: larger; extend superiorly
- Utricular cyst: smaller; communicate with urethra; ↑ hypospadias
- Ejaculatory duct cyst: acquired; due to obstruction
- Eccentric:
- Cystic prostatitis/ carcinoma
- Cystic BPH
- DDX = seminal vesicle cysts → unilateral; ↑ ipsilateral renal agenesis (= Zinner syndrome) > cystic renal disease (APKD), renal ectopia, duplication, ectopic renal insertion
Prostate Carcinoma
- Clinical: # 2 male CA; enlarged gland with nodules; periprostatic stranding; regional nodes; direct extension to seminal vesicles, bladder; mets to axial skeleton
- Radiographic: hypoechoic; ↓ T2 lesions in peripheral gland (DDX = prostatitis; fibrosis; hemorrhage)
Staging
- Stage A: nonpalpable
- Stage B: confined to prostate
- Stage C: capsular involvement
- 1: invasion
- 2: penetration
- 3: seminal vesicles
- Stage D: metastases
- D1: pelvic LN
- D2: bone; distant LN
- Treatment: Stage A/B → radical prostatectomy +/- XRT; Stage C/D → hormone therapy +/- XRT
Peritoneal Cavity, Vessels, and Nodes
Fluid in peritoneal cavity
- Ascites: serous; due to CHF, cirrhosis, hypoproteinemia, venous obstruction; accumulates in greater peritoneal space; density = 10-15 HU
- Exudative ascites: pancreattis → accumulates within lesser sac; peritonitis; bowel perforation
- Hemoperitoneum: density > 30 HU; “sentinel bleed” → accumulates at site of hemorrhage
- Pseudomyxoma peritonei: due to appendiceal mucocele or mucinous cystadenocarcinoma of the ovary (> urachal/ endometrial CA); peritoneum filled with gelatinous mucin; Ca2+
Pneumoperitoneum
- due to bowel perforation, pneumothorax, or mechanical ventilation
Peritoneal tumors
- Peritoneal carcinomatosis:
- Etiologies: ovarian, pancreatic, gastric, and colon carcinoma
- Radiographic: malignant ascites; tumor nodules/ Ca2+ → bowel wall nodularity; mesentery; “omental cake”; pouch of Douglas (“Blumer’s shelf); adnexa/ ovaries (Krukenberg tumor)
- Peritoneal (cystic) mesothelioma: 20-40% in abdomen; ↑ women 30-40 years; irregular thickening of peritoneal surfaces; multilocular cysts; ascites; bowel compression without obstruction
- Mesenteric lipodystrophy (= retractile mesenteritis): fat-density mass with tethering/ kinking/ angulation of adherent bowel loops
Abscess
- Clinical: complications of trauma or surgery; pancreatitis; bowel perforation; commonly located within pelvis, subhepatic and subphrenic spaces
- Radiographic: loculated fluid collection; thickened walls; gas; thickening of fascia; obliteration of fat planes; ascites; pleural effusions
DDx for cystic abdominal masses
- Abscess
- Loculated ascites
- Pancreatic pseudocyst
- Ovarian cyst/ tumor
- Cystic teratoma: fat, water, Ca2+
- Enteric duplication cysts: lined by GI mucosa
- Lymphocele: complication of surgery / trauma
- Cystic lymphangioma: mesenteric / omental
DDx for pelvic cystic masses
- Ectopic pregnancy: adnexal/ tubal ring
- TOA: tubo-ovarian abscess
- Endometrioma
- Ovarian neoplasms
- Ovarian cysts
- Extra-GU origin: abscess; urinoma; duplication/ mesenteric cyst; etc.
Lymph nodes
- Pathology: lymphadenopathy: > 10 mm in abdomen and pelvis; > 6 mm in retrocrural and porta hepatis regions
- Hodgkin’s lymphoma: 40% of total; contiguous spread
- Non-Hodgkin’s lymphoma: 60% of total; noncontiguous spread; ↑ GI involvement
DDx for hypodense intra-abdominal/ retroperitoneal LAD
- Infection: MAI > TB (↑ AIDS), histoplasmosis
- Whipple’s disease: glycogen deposition
- Tumors: lymphoma (post-therapy); nonseminomatous testicular CA; mucinous adenoCA (rare)
Trauma
- Hemoperitoneum: density (30-45) HU; (60-80) HU → active bleeding (> 100 HU with contrast); “sentinel clot” → adjacent to injured organ (> 60 HU); free intraperitoneal contrast → bowel/ bladder perforation
- Pneumoperitoneum: perforated viscous; PTX; mechanical ventilation; post-op
- Subcapsular hematomas: crescentic → flatten parenchyma
- Lacerations: jagged, linear low density areas
- Intraparenchymal hematomas: rounded, low density areas
Retroperitoneum
Retroperitoneal fibrosis
- ST-encasement of retroperitoneal vessels/ ureters without anterior displacement (DDX = lymphoma); prominent enhancement
- Drugs: methylsergide; hydralazine
- Lymphoma
- Metastases: lung; breast; carcinoid
- Other: AAA; trauma; surgery; instrumentation
- Ormond’s disease: idiopathic
DDx for retroperitoneal masses
Malignant
- MFH (#1)
- Liposarcoma (#2)
- Other: leiomyosarcoma; metastases; RCC/ adrenal extension
Benign
- XGP
- Neural tumors
- Lymphangioma; hamangioma; lipoma
- Teratoma (dermoid)
Retroperitoneal Fibrosis
- Associated w/
- aortic aneurysms
- inflammatory bowel dz
- urinomas
- retroperitoneal hematomas
- aortic and iliac graft procedures
- infections
- ergot alkaloids
- sclerosing cholangitis
- fibrosing mediastinitis
Waterhouse-Friderichsen syndrome
- massive, usually bilateral, hemorrhage into the adrenal glands caused by fulminant meningococcemia
Low-density Retroperitoneal Nodes
- Neoplastic
- Testicular (particularly teratocarcinoma)
- Epidermoid carcinoma of GU tract
- Lymphoma
- Leiomyosarcoma
- Infectious
- Whipple's Dz
- MAI
gu.txt · Last modified: 2024/07/16 15:47 by 127.0.0.1