interventional
Table of Contents
Post-Traumatic Vascular Injury
CXR Signs
- wide mediastinum
- filling in of AP window
- depressed L mainstem
- rightward displacement of trachea or NG tube
- L apical cap
- L effusion
- L upper rib fxs
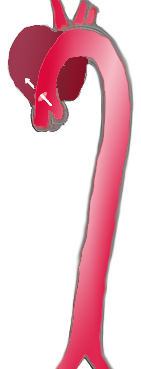
Most Common Locations for TAI
- Aortic root
- Isthmus
- Aortic hiatus
Classification of Dissections
Aortic Aneurysms
- CT signs of impending rupture
- high attenuation crescent between intraluminal thrombus and the wall
Types of Endoleaks
- Type 1 - bad seal @ prox/distal end
- treatment is emergent
- Type 2 - endoleak via IMA or lumbar collaterals
- Type 3 - leak thru internal seal
- Type 4 - porosity of graft
- resolves spontaneously
- Type 5 - endotension
- sac not getting smaller, but no leak
Takayasu's
- dilation or irregularity of the ascending aorta
- narrowing of the descending artery
- long stenoses or occlusions of arch vessels (especially the subclavian)
- CT/MR show enhancement of the artery wall in the acute phase
- angioplasty and stent should be delayed until the disease is inactive if possible
- Type 1 → stenoses of aortic arch and branch vessels
- Type 2 → descending thoracic and abdominal aorta + abdominal branches
- Type 3 → aortic arch plus abdominal aorta
- Type 4 → pulmonary artery and aorta
Giant Cell Artieritis
- affects older women, and usually involves the temporal artery
- involves the distal subclavian or axillary arteries, but not the brachiocephalic, common carotids or proximal subclavians
- lesions are long and smooth
DDx Midaortic Stenosis
- Midaortic stenosis
- noninflammatory nonatheromatous vascular d/o
- can cause renal artery stenosis
- Takayasu's
- Radiation induced
- Neurofibromatosis
Aortic Occlusion
Collateral Pathways
Contraindications
- recent surgery (intracranial, abdominal, or thoracic)
- recent GI bleed
- recent stroke or CNS neoplasm
- recent major trauma
- pregnancy
- severe HTN
- bleeding diathesis
- infected thrombus
TIPS
Indications
- variceal bleeding that cannot be treated medically (acute or chronic)
- intractable ascites
Contraindications
Absolute
- polycystic liver disease
- severe R heart failure
- severe hepatic failure
Relative
- severe hepatic encephalopathy
- hypervascular liver tumor
- portal vein thrombosis
- severe acute infection
Technique
- Do u/s first to assess PV patency, flow direction, status of hepatic veins, degree of ascites, and eval for liver tumor
- Check coags and correct w/ FFP
- Broad spectrum antibiotics
- 10Fr sheath RIJ and assess RA and IVC pressures
- Measure wedged hepatic vein pressure which will equal PV pressure, subtract the IVC pressure to get gradient
- Insert needle
- Opacify the portal vein via a wedged contrast injection
- Stick the needle anteromedially into the right portal vein
- Needle is then withdrawn a bit until you get blood back
- Inject contrast to check your position
- Advance a guidewire into the PV and then to the splenic vein or SMV
- Dilate the parenchymal track with a 10mm balloon
- Place 10 or 12 mm Wallstent so that one end is within 3 cm of the portal bifurcation, and the other within 3cm of the IVC
- Dilate tract with a 10mm balloon
- If gradient remains (>12mm Hg), redilate w/ 12mm balloon
- If gradient persists, can employ parallel stent or embolize varices
Paget-Schroetter Disease
- Best seen w/ provocative maneuver such as hyperabduction
Causes
- cervical rib
- congenital fibromuscular bands
- 1st rib anomalies
- muscle hypertrophy
- clavicle fxs
Management
- If severe or pt has embolization, then correction of underlying abnormality is recommended
Colonic bleed
- Causes of lower GI bleed:
- diverticular dz
- angiodysplasia (dilated submucosal veins and capillaries in the bowel wall)
- post biopsy or polypectomy
- tumors
- polyps
- IBD
- ischemia
- Patients with a positive Tc RBC or SC scan should undergo angio
- Sensitivity:
- angio - 0.5cc/min
- Tc RBC - 0.1cc/min
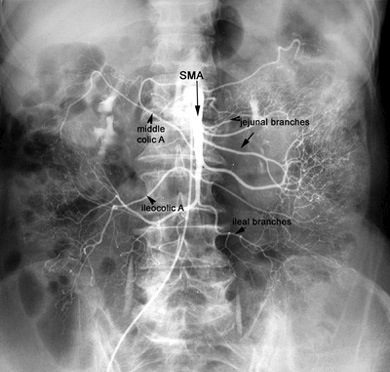
- Most likely vessel, based on nucs scan, should be injected 1st
- Otherwise SMA then IMA, and if both negative, then celiac
- In angidysplasia, a bleeding vessel is usually not seen
- instead, you see early venous drainage from one portion of the bowel, or a tram track sign from simultaneous opacification of a feeding artery and draining vein
- Treatment:
- vasopressin - 0.2 units per minute
- after 30 minutes a repeat angiogram is done, the infusion is continued at that rate with the pt in ICU
- if persists, increase to 0.4u/min and repeat angio in 30 minutes
- if still bleeding, need to pursue other methods
- rebleeding is common
- Contraindications: severe coronary artery dz, severe HTN, dysrhythmias, bleeding at sites with a dual blood supply, bleeding directly from a large artery (eg spl artery aneurysm) and after embolotherapy
- Side effects: bowel ischemia, angina, arrythmia, HTN, bradycardia, and allergy
- embo - performed with macrocoils or microcoils and gelfoam
- embo usually does not work long term for angiodysplasia or AVM, these will require surgery
- placed distally in the arcades proximal to the bleeding vasa recta to minimize intestinal ischemia
- inject the proximal vessel to make sure there is no bleeding thru collaterals
- complictions include bowel infarct <20%
Pulmonary Embolism
- Primary finding - intraluminal filling defect at least partly surrounded by contrast
- Secondary signs - vessel cutoff, regional hypoperfusion, pruning of vessels, slow flow, and filling of collaterals
Technique
- check for LBBB & use pacer if present
- also check u/s for groin clot
- check PA pressures before injecting main PA; cut back on injection if pressures are elevated
Transhepatic Cholangiogram
Procedure
- Start w/ antibiotics to include gram negative coverage - one hour prior to any biliary work
- Right sided approach:
- 22G Chiba needle is placed in the midaxiallry line below the 10th rib (to avoid the pleura)
- fluoro is used to check the position of the pleura in full inspiration, so that it may be avoided
- needle is passed over a rib, to avoid injury to the nerves and vessels which run on the undersurface
- needle is directed toward a plane parallel to the table top aimed toward T11
- remove the stylet and inject 0.1cc of 60% strength contrast while slowly retracting the needle
- when contrast fills a tubular structure and stays there, you are likely in a bile duct, and you should remove 5-10 cc of bile and send for gram stain and culture
- then inject an additional 5-10cc contrast to confirm and determine duct diameter and location relative to porta hepatis
- Left sided access:
- from a left subcostal approach in the epigastrium
- US is used to access a bile duct while avoiding artery and portal vein
- Treatment:
- pass a 0.018 wire thru the chiba needle you used for the THC, then exchange for a .038 wire, and advance a catheter over that wire
- a dominant proximal stricture can be angioplastied
- stents can be used for malignancy b/c the pts life expectancy is short and the stent will likely last as long as the pt needs
- for benign dz, stents should only be used for pts who are not operative candidates and who failed angioplasty
- a wallstent is the stent of choice
IVC Filter
Contraindications
- IVC thrombosed
- pregnancy (clot may come from ovarian veins)
- place suprarenal filter
Nephrostomy
Technique
- check labs; stop anticoagulants
- prophylactic antibiotics 1hr preprocedure (ancef 1g and gentamycin 80mg or specific to the organism)
- place pt prone and select puncture site (4 fingers from midline, just below 11th rib)
- start by puncturing collecting system with a 22G Chiba needle and opacifying collecting system
- aspirate urine for culture and remove urine before injecting contrast to minimize sepsis risk
- choose best entry site under fluoro:
- for simple decomression, it is safest to puncture a lower pole calyx b/c that has the lowest risk for PTX
- if ureteral stent placement is planned, then go for an interpolar calyx to get an easier angle to get the catheter down the ureter
- puncture at least 12 cm lateral to midline in order to avoid going thru paraspinal muscles
- puncture a posterior calyx (know posterior b/c seen en face in AP plane, or can inject air) with an 18G needle
- posterolateral approach, with needle angled 40 degress from vertical is best (Brodel’s avascular line)
- if infected, initially just decompress, do not manipulate more until infection is treated
- place a stiff amplatz .035 down into ureter
- the tract is dilated, and a 10 fr pigtail is placed over the .035 wire and locked into position by forming the pigtail
- secure to skin with adhesive dressing or suture.
Signs of Leg Ischemia
- hair loss
- nail changes
- purple toes
- skin loss
- ulcers
Sources of Hemoptysis
Bronchial Artery
- Cystic Fibrosis
- Infection
- Bronchiectasis
- Tumor
Technique
- place the catheter deep into the abnormal bronchial artery
- if you can not get deep with your initial catheter, place a coaxial microcath thru it to go out deeper
- findings in pts with a bronchial artery bleed include eenlarged bronchial artery, hypervascularity, parenchymal stain, amd bronchial to pulmonary artery shunting
- contrast extrav is not usually seen, and is not necessary for treating
- look for the small branches to the anterior spinal artery which arise form the proximal portion of the vessel and take a hairpin turn going 1st superior and then inferior toward midline
- if there is a spinal artery branch, some people wont embolize, but some will embo if they can get the catheter well beyond the branch
- embo agent is PVA (medium sized particles) or gelfoam
- if no bronchial or collateral bleeding source is found, then you have to inject the pulmonary arteries
Pulmonary Artery
- Rasmussen Aneurysm
- Pulmonary AVM
- Unlike other AVM's, as there is no real nidus
- Therefore, it is the only AVM where you embolize the feeding vessel
- Use coils!
- PA Pseudoaneurysm
TPA Thrombolysis
- Dose = 0.5 mg/hr infusion
- No bolus needed
Contraindications
- Motor weakness in extremity
- Do not want to perfuse dead tissue
Popliteal Artery Disease (ABCDE)
- Atherosclerotic disease / Aneurysm
- Buerger's disease
- corkscrew vessels
- Baker's cyst
- Cystic adventitial disease
- cysts in vessel wall on IVUS
- Dissection
- Entrapment
- induced by plantarflexion or forced dorsiflexion of foot
- caused by abnormal relationship with medial head of gastrocnemius
General Technique
Seldinger
- 18G - .035 wire
- 22G - .018 wire
Stenting
Good Locations for Covered Stents
- SFA
- TIPS
- Lacerated vessel
Embolization
- always use medium size particles
- 500-700 microns
Vasopressin
- Done from origin of vessel
- Usually only if embo is not possible
TPA Infusion
- place multisidehole catheter across occlusion
- 2mg initial TPA bolus
- then infuse 1mg/hour
- f/u angiogram in 12hrs
- treat residual stenosis w/ angioplasty
- give heparin prior to thrombolysis
- 5000U bolus then 1000U/hr infusion
Anatomy
Celiac
SMA
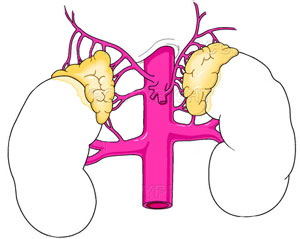
Adrenal
Run-off
interventional.txt · Last modified: 2024/07/16 15:47 by 127.0.0.1